UCSF Dept of Family and Community Medicine Grand Rounds
Held every first Friday of the month from 12-1pm.
How do I participate in the upcoming Grand Rounds?
To be added to the invitation list and receive the link please email: F[email protected]
To view past presentations please visit our playlist: FCM Grand Rounds playlist
Upcoming Presentation
April 4, 2025 - Walking the Talk: Decolonizing Global Health & Health Equity Education in Uncertain Times

Jessica Evert, MD
Dr. Jessica Evert, UCSF Department of Family and Community Medicine Clinical Professor and Global Medical Director of Child Family Health International, a leading non-profit in Global Health education, will present a sweeping perspective on decolonization of Global Health and Health Equity education. Grounded in research and evidence-based theories of change, she will dive into the theoretical and applied frameworks at the intersections of decolonization, ethics, and educational pedagogy. In a moment when US international engagement and development is experiencing dramatic shifts at the federal level, Dr. Evert will discuss the essential roles of academia, civil society, the private sector, and other stakeholders. She will detail strategies to maintain momentum in Global Health and international engagement while the US faces deep divisions in our approach to health equity at home and abroad, while not comprising progress over the past 20 years to optimize authenticity and rigor within Global Health education and practice.
Dr. Jessica Evert straddles international education and the medical profession. She served as CFHI Executive Director from 2013-2021 and is currently CFHI’s Global Medical Director. She oversees CFHI safety and risk management, thought leadership, publications, and advocacy. She has co-authored dozens of articles and texts focused on best practices for student and faculty engagement in global health. Dr. Evert is a Faculty in the Department of Family and Community Medicine at the University of California, San Francisco, where she instructs in Global Health and community-based underserved care and helped develop, as well as completed, the Global Health Clinical Scholars residency track. Dr. Evert is a graduate of the Ohio State University College of Medicine and is a longtime advocate for health-related international education quality and ethical standards. She is the author and editor of multiple chapters, articles, and books on global health with a focus on education, ethics, and asset-based engagement, including the seminal texts, Global Health Experiential Education: From Theory to Practice, Developing Global Health Programming: A Guidebook for Medical and Professional Schools, 2nd Ed, Global Health Training in Graduate Medical Education, 2nd Ed and Reflection in Global Health: An Anthology. She helped develop the Forum on Education Abroad’s Standards for Health-Related Undergraduate Programs. She serves on the Consortium of Universities for Global Health’s Education Committee, as well as multiple other leadership bodies over 2 decades. Dr. Evert is a recipient of the Global Health Education Consortium’s prestigious Christopher Krogh Award for her dedication to underserved populations at home and abroad. Dr. Evert’s research and advocacy areas of focus are the ethics of global educational engagement, competency-based international education, health disparities, asset-based programmatics and reflection. Dr. Evert is a practicing physician in the Western United States focusing on hospital medicine and palliative & supportive care.
Past Presentations
March 7, 2025 - Innovation in Primary Care as a Solution for Population Health
February 7, 2025 - The Fundamental Importance of Social Insurance for Health Equity
December 6, 2024 - Skills for Systemic Change: The Potential of Primary Care Health Policy Education
November 1, 2024 - A Case Study in Structural Racism and Urbanism: The Neglect of Valley Fever
October 6, 2024 - The Joys and Impact of Family Medicine in Birthing Care
August 2, 2024 - Advancing Healthcare and Economic Development in Indian Country
April 5, 2024 - The Changing Landscape of Primary Care: a Canadian perspective
March 1, 2024 - Community Grand Rounds: Equitable Relationships for Equitable Health Outcomes
February 2, 2024 - Preparing the Next Generation of Leaders and Change Agents
November 3, 2023 - Health Services and Outcomes Research to Support Quintuple Aim in Primary Care
September 1, 2023 - Aging and End of Life Care in an Incarcerated Setting
September 2, 2022 - Dr. Ayanna Bennett - Moving from Intention to Action on Health Equity
January 7, 2022 – Dr. Garen Wintemute – “Firearm Violence: Where We Stand, What We Can Do”
May 7, 2021 – Dr. Rita Hamad - “Social Policies to Address Health Inequities: Harder Than It Looks”
March 7, 2025 - Innovation in Primary Care as a Solution for Population Health

Kameron Leigh Matthews, MD, JD, FAAFP
Primary care serves as the foundation for scaled population health improvement. Dr. Matthews will emphasize the principles of primary care as the building blocks to improved quality, equity, and cost at scale. She will share models of advanced primary care that move beyond individual patient care and seek to achieve the quintuple aim through integration and team-based approaches.
Dr. Kameron Leigh Matthews is the Chief Health Officer of Cityblock Health, a transformative, value-based healthcare provider integrating medical, behavioral, and social services for Medicaid and dually eligible and low-income Medicare beneficiaries. A board-certified Family Physician, Dr. Matthews has focused her career on underserved and vulnerable communities, having held multiple leadership roles in correctional medicine, federally qualified health centers, managed care, and other non-profit organizations, as well as led transformational efforts in Veterans Health Administration including the implementation of the MISSION Act of 2018 and the EHR modernization effort.
February 7, 2025 - The Fundamental Importance of Social Insurance for Health Equity
Seth Berkowitz, MD, MPH
This talk will draw from the recent book Equal Care: Health Equity, Social Democracy, and the Egalitarian State. It will describe the relationship of income distribution to health outcomes, and discuss how to design, implement, and finance income support policy that can improve population health and health equity.
Dr. Berkowitz is an Associate Professor of Medicine and Section Chief for Research at the University of North Carolina at Chapel Hill School of Medicine in the Division of General Medicine & Clinical Epidemiology. He is a general internist and primary care doctor, and completed the University of California San Francisco Primary Care Internal Medicine residency program. He studies the relationship between health-related social needs, such as food insecurity, and health outcomes. He is the author of the recent book Equal Care: Health Equity, Social Democracy, and the Egalitarian State, which examines how public policy can improve population health.
January 10, 2025 - UCSF-Community Partnership for local Chronic Disease Equity (Part 2): Lessons, Challenges and Opportunities of SF’s Soda Tax years






beginning top row l to r
Anisha Patel, MD, MSPH, MSHS - Marianne Szeto, MPH - Jonathan Butler, PhD, MDiv
Joi Jackson-Morgan - Abby Cabrera, MPH - Roberto Vargas, MPH
Hear how UCSF, community and City partners advanced “Water Equity” and leveraged the SF Soda Tax revenue to make measurable improvements to community health. Hear about promising opportunities to re-engage with community leaders, and to save the imperiled resource that is the SF Soda Tax.
Anisha I. Patel, MD, MSPH, MSHS, is a Professor of Pediatrics and Epidemiology and Population Health at Stanford. She is the Director of Community-Engaged Research at Stanford’s Maternal and Child Health Research Institute and an Associate Dean of Research at Stanford’s School of Medicine. She directs the Partnerships for Research in Child Health Lab, which partners with communities on research to address inequities in child health with a focus on the prevention of chronic diseases. She has published extensively and her innovative scholarship has been highlighted by media, including CNN, National Geographic, and NPR. Her work has been funded by the National Institutes of Health, the Robert Wood Johnson Foundation (RWJF), and the W.K. Kellogg Foundation. She has served on numerous committees led by the Centers for Disease Control and Prevention, American Heart Association, and RWJF. Her scholarship has influenced local and federal child health policies. Dr. Patel has received numerous awards, including the American Academy of Pediatrics Outstanding Achievement Award in the Application of Epidemiologic Information for Child Health and the Sidney S. Chipman Award in Maternal and Child Health from the University of North Carolina, Chapel Hill (UNC-CH). She is currently an Executive Leadership in Academic Medicine program fellow. Dr. Patel has received a K24 Midcareer Investigator Award in Patient-Oriented Research from the National Heart Lung and Blood Institute that supports her mentoring of trainees. She works clinically in general pediatrics at the Gardner Packard Children’s Health Center, a federally qualified health center affiliated with Stanford.
Marianne Szeto, MPH, is a public health professional with over 16 years of experience in community health education, program management, and stakeholder engagement. Currently serving as the Acting Chronic Disease Prevention Manager in the Community Health Equity and Promotion Branch of the San Francisco Department of Public Health, Marianne leads the Healthy Eating Active Living (HEAL) Team and provides backbone support for the Shape Up SF Coalition and the Sugary Drinks Distributor Tax Initiative. Marianne’s efforts have been instrumental in shaping the San Francisco soda tax, where she implemented education and awareness campaigns and trained community partners on the health impacts of sugary drinks and industry tactics. She holds a Master of Public Health from San Jose State University and a Bachelor’s in Classics from UCLA.
Jonathan Butler, Phd, MDiv is the associate director of the Black Health Initiative at the University of California at San Francisco (UCSF) and a social epidemiologist in the Department of Family and Community Medicine. He is also a consultant at UCSF's Clinical & Translational Science Institute (CTSI). He serves as a mayoral appointee and inaugural chair of the San Francisco Homelessness Oversight Commission, vice chair of the SF Interfaith Council, and vice president of the NAACP SF branch.
Joi Jackson-Morgan is the Executive Director at 3rd Street Youth Center & Clinic. Joi’s most important contribution to 3rd Street has been her ability to combine insight into the history of the neighborhood with both her formal education in public health and her professional experience. She was born and raised in Bayview Hunters Point, the Southeast sector of San Francisco. She has worked as a math and science teacher at several Bay Area junior high and high schools and as a research assistant on community-based health studies. Joi’s broad experience and education in health and education inform her approach to working with individual youth and the community as a whole. Under Joi’s leadership, 3rd Street has experienced exponential growth fortifying its standing as a leader in housing and behavioral health services for young people, and recently opened San Francisco's first TAY Navigation Center for young adults experiencing homelessness. Joi is committed to centering the importance of racial equity and justice to end youth homelessness. Joi is currently the Co-Chair of the Black/African American Health Initiative on Sexually Transmitted Infections (BAAHISTI). She received her masters of public health from Charles R. Drew University of Medicine and Science and her Bachelors of Science in Biology at California State University-East Bay.
Abby Cabrera, MPH is an Associate Director of Research and Community Engagement at UCSF’s Center for Excellence in Primary Care and the CTSI Community Engagement Program. Abby has over 10 years of experience in public health research aimed at improving health equity and decreasing health disparities through community engagement programs and primary care research. Her experience ranges from managing community-based participatory research projects, curriculum and training development for COVID-19 vaccine outreach, community benefit programs and activities for hospitals conducting community health needs assessments, qualitative research, and coalition evaluation addressing the social determinants of health. Abby is honored to serve as the Sugary Drinks Distributor Tax Advisory Committee (SDDTAC) Co-Chair and brings her passion for helping communities improve their health outcomes and lived experiences.
Roberto Ariel Vargas, MPH is Associate Director for the Center for Community Engagement and Senior Staff at the Community Engagement and RAGE Programs of UCSF’s Clinical and Translational Science Institute. Vargas has helped shape health policy and practice at the municipal and national levels on chronic disease prevention and cancer care, primarily by leveraging the expertise of UCSF scientists and community health advocates. Vargas served on the National Cancer Institute’s National Council of Research Advocates, the board of the Central American Resource Center (CARECEN) & co-chair of the SF Sugary Drinks Distributor Tax Advisory Committee & is currently on the board of the American Heart Association Bay Area & Instituto Familiar De La Raza. Prior to joining UCSF’s Department of Family and Community Medicine nearly 20 years ago, Vargas led community-based nonprofit organizations and school-based health and social service programs. As Director of the Real Alternatives Program Collaborative, Vargas began as a partner to UCSF on community-engaged research projects, and then as a community advisor to UCSF’s first community-university partnership program.
December 6, 2024 - Skills for Systemic Change: The Potential of Primary Care Health Policy Education


Kevin Grumbach, MD - Eushavia Bogan - Kweku Djan



Melissa Ma - Ananya Somasekar - Zakiyyah Winston - AC Fernandez
This talk will discuss the mission and impact of the Primary Care Health Policy Scholars Program. The Primary Care Health Policy Scholars Program’s aims to support students’ development of primary care health policy knowledge, build critical social theory frameworks, and practice the skills needed to create systems change. Through popular education, policy-based praxis, and coalition building with patients, healthcare workers, and policy makers, the program seeks to offer tangible pathways for students to get involved in the politics of health. We believe that medical students are integral to dismantling the current profit-driven and fragmented U.S. healthcare system. Therefore, we aim to equip future physicians with the community, knowledge, and tools to advocate for robust primary care services and equitable, whole person healthcare for all. We hope that collectively, through this program and coalition building, we can generate greater medical student interest and advocacy in primary care as well as uplift student voices, leadership, and passion in social movements for a more just healthcare system.
Kevin Grumbach, MD is Professor of Family and Community Medicine at the University of California, San Francisco. He served as Chair of the UCSF Department of Family and Community Medicine from 2003 to 2022 and is a Founding Director of the UCSF Center for Excellence in Primary Care and Director of the Community Engagement Program for the UCSF Clinical and Translational Science Institute. Dr. Grumbach currently serves on the California Health Workforce Education and Training Council and the Investment and Payment Work Group for the California Office of Health Care Affordability, and co-chairs the California Academy of Family Physicians Task Force on Primary Care for All. He was elected to the National Academy of Medicine in 1997 and currently serves on the NASEM Standing Committee on Primary Care. He cares for patients at the family medicine practices at San Francisco General Hospital and UCSF Health.
Eushavia Bogan is a third-year medical student at UCSF and co-creator of the UCSF Primary Care Health Policy Scholars Program. Prior to matriculating at UCSF, Eushavia received a BA from Vassar College in Environmental Studies in 2013. After graduating they returned to their native Brooklyn, New York to work as a community organizer and urban farmer. Their work focused on collaborating with neighborhood stakeholders to advocate for food sovereignty and improve community well-being in their native Brooklyn, NY. Eushavia intends to apply the knowledge gained from these experiences to their work as a family medicine doctor and co-conspire with communities to build public health systems that center equity and collective care.
Kweku Djan is a fourth-year medical student here at UCSF and is currently pursuing a one-year Masters of Public Health at UC Berkeley. He grew up in Sacramento, CA and completed his undergrad at Yale University. He is planning to apply into Family Medicine and pursue a career practicing primary care among underserved communities.
Melissa Ma is a second-year medical student at UCSF. She is a Bay Area native and plans to pursue family medicine. She is drawn to family medicine for its important role in prevention, its holistic approach to care, and the capacity to build longitudinal relationships with patients. She has a strong interest in health policy and contributing towards systemic change to improve healthcare access and equity.
Ananya Somasekar is a second-year medical student at UCSF. Her background is in public health, where her work and research were primarily focused on housing insecurity, environmental health, and health equity. She is passionate about primary care and hopes to pursue a career in family medicine or pediatrics.
Zakiyyah Winston is a third-year medical student at the University of California, San Francisco interested in family medicine, adolescent health, reproductive health, integrative medicine, and primary care policy. Zakiyyah earned a B.S. in Biology with a minor in Health Studies from Haverford College in 2022. Since college, she has approached all of her work with a health equity and justice lens with a particular focus on the experience of Black people in healthcare. At UCSF, she's dedicated time to uplifting the next generation of racial and ethnic groups underrepresented in medicine through her time as Mentorship Chair with the SNMA and as Mentor Lead with Health Link—a year-long program for first-generation college-bound high school students in the Bay Area. Outside of school, Zakiyyah enjoys cooking, curating playlists, and hiking!
AC Fernández is an MS4 applying into Emergency Medicine. Her research is dedicated to understanding the impact of wildfire smoke exposure on pregnancy outcomes, especially in vulnerable populations. She joined the inaugural class of health policy scholars in order to learn more about equalizing the healthcare system in the United States and to collaborate with her peers to help increase patient’s access to care.
November 1, 2024 - A Case Study in Structural Racism and Urbanism: The Neglect of Valley Fever

Nancy J. Burke
Coccidioidomycosis, colloquially referred to as Valley Fever, affects residents in the southwestern United States, northern Mexico and areas of South America. An estimated 150,000 people in the United States become infected annually via inhalation of spores from the soil-dwelling fungi. This can lead to chronic lung infection, meningitis, or death. Southwestern states are experiencing among the highest incidence rates of coccidioidomycosis ever recorded. Large construction projects, such as the creation of solar farms, and earthquakes that disturb the soil increase risk of infection. Administrative reviews of statewide hospitalization rates show that 25,000 individuals were admitted to the hospital in California between 2000-2011 with Valley Fever-associated issues, at an estimated cost of $2.2 billion. While most cases resolve spontaneously, up to 40% are severe enough to require antifungal treatment and many spread beyond the lungs. No new treatments for coccidioidomycosis have been approved in the United States in nearly 40 years; the number of investigators studying the disease is very small and there is little pharmaceutical company interest in developing treatments. The fact that the areas most affected in California are also the poorest communities in the state, and home to the state’s prisons, may also have influenced the lack of attention to this disease. I explore the social, racial, and regional stratifications that inform its neglected status.
Nancy J. Burke is Professor of Public Health and Anthropology and John D. and Catherine T. MacArthur Foundation Endowed Chair, University of California, Merced. She also serves as Co-Director of the UC-Cuba Academic Initiative. Her current research includes projects focused on ageing in Cuba, politics and poverty in relation to Valley Fever (coccidioidomycosis) research, and the role(s) of community organizations in COVID-19 response in California’s Central Valley.
October 6, 2024 - The Joys and Impact of Family Medicine in Birthing Care











beginning top row l to r
Christine Pecci, MD - Audrey Arai, MD - Renée Betancourt, MD - Gabriel Flaxman, MD
Robin Linscheid, MD - Rebecca McEntee, MD - Elizabeth Kyle* Meehan, MD - Leah Suárez-Abraham, MD
Hannah Watson, MD - Amanda Wong Kim, MD, MPH - Nicole Person-Rennell, MD, MPH, FAAFP
Family physicians are uniquely equipped to address care gaps that contribute to our National Maternal Health Crisis. In this presentation, faculty in surrounding family medicine residency programs and former UCSF FCM graduates will share successful models of care and training in family medicine obstetrics. We will share the impact of our work on the communities we serve, and how it enhances our joy as family physicians.
Christine Pecci, MD is a Clinical Professor at the UCSF Department of Family and Community Medicine. She practices full-scope family medicine, including primary care, inpatient medicine, and labor and delivery. She also is part of the obstetrics leadership at the John Muir Family Medicine residency program and provides birthing care for patients from La Clinica De La Raza, an FQHC based in Oakland . Christine completed an OBGYN internship and an obstetrics fellowship in addition to her family medicine residency. She previously was faculty at Boston University and Lawrence Family medicine residencies before joining UCSF.
Audrey Arai, MD is a family medicine doctor on faculty with the John Muir Family Medicine Residency Program in Walnut Creek, California where she is Obstetrics rotation director. She completed residency at UCSF followed by the Family Practice in Obstetrics Fellowship at Santa Clara Valley. She is also an Assistant Professor at UCSF where she attends on Labor and Delivery.
Renée Betancourt, MD is an Associate Professor of Clinical Family Medicine and Community Health at University of Pennsylvania and Vice Chair for Education and Diversity Equity and Inclusion for the department. She trained at the UCSF Family and Community residency and then served as chief resident year from 2011-2015. She practices the full scope of Family Medicine including gender-affirming care, substance use care, chronic diseases, routine GYN care, contraception and family planning, pre-natal care, and obstetrics.
Gabriel Flaxman, MD is faculty at the Kaiser Permanente Napa-Solano Family Medicine Residency. He trained at Santa Rosa Family Medicine residency and then completed an OB fellowship. He practices full scope family medicine including operative obstetrics. He oversees the obstetrics and women’s health curriculum and won a teaching award in 2018.
Robin Linscheid, MD is Clinical Associate Professor and UCSF Fresno where she was born and raised. She has a special interest in women’s health, obstetrics, pediatrics, harm reduction, substance use treatment and trauma informed care. As part of the Maternal Child Adolescent Health division of Fresno County Public Health she has put into practice her passion for advocacy and improving the health of the Central Valley, especially in our most resource poor communities. Dr. Linscheid is chair of Fresno County’s Perinatal Substance use taskforce and FIMR board and core faculty at UCSF Fresno Family and Community Medicine Residency. She is also District VI Director for the California Academy of Family Physicians.
Rebecca McEntee, MD is a primary care provider at La Clinica de la Raza's San Antonio Neighborhood Health Center and Davis Pediatrics Clinic. She is also faculty in the Lifelong Medical Care Family Medicine Residency Program and serves as the curriculum director for obstetrics and gynecology. Additionally, Dr. McEntee is an Assistant Clinical Professor in the UCSF Family and Community Medicine Residency Program where she trains family physicians in abortion care. She is a graduate from the UCSF Family and Community residency program.
Elizabeth Kyle* Meehan, MD is an Associate Program Director of University of Arizona Family and Community Medicine Residency. She previously was the Program Director for University of Arizona South Campus Family Medicine Residency. She graduated from UCSF Family and Community Medicine Residency in 2013, and served as Chief Resident until 2014. She practices full-spectrum Family Medicine caring for patients of all ages in the outpatient clinic, adult inpatient hospital service, and on their Maternal Child Health Service (providing labor and deliver, postpartum and newborn care). She is an attending provider at University of Arizona Mobile Health Prenatal Program where uninsured pregnant persons receive free prenatal and postpartum care. After residency, she completed the Andrew Weil Center for Integrative Medicine (AWCIM) Fellowship and is the Associate Director of Integrative Medicine in Residency for AWCIM.
Leah Suárez-Abraham, MD is a family physician at the FQHC Salud Para La Gente and practices Obstetrics at Watsonville Community Hospital, where she coordinates resident OB-Peds rotations and is the Director for Curriculum and Didactics. Dr. Suárez-Abraham trained at Ventura Family Medicine Residency, and completed a fellowship in Maternal Child Health. After fellowship, she spent two and a half years in Santiago Atitlán, Guatemala, where as a medical volunteer, she assisted in the re-opening of the Hospitalito Atitlán and later served as its Chief of Staff. Subsequently, she moved to Chicago where she served as faculty for the West Suburban Medical Center Family Medicine Residency Program and became Co-Director of the PCC Community Wellness Center Maternal Child Health Fellowship.
Hannah Watson, MD is the Maternity Care Director at the Sutter Santa Rosa Family Medicine Residency and the Chair of the Department of Family Medicine at Sutter Santa Rosa Regional Hospital. She completed the University of New Mexico Maternal, Child and Reproductive Health Fellowship where her research focused on perinatal substance abuse and group prenatal care. She has worked at Santa Rosa Community Health since 2017, where she takes surgical Ob call and practices primary care and addiction medicine.
Amanda Wong Kim MD, MPH, is a Clinical Assistant Professor at University of Washington - Valley Family Medicine Residency. She completed a surgical high-risk obstetrics fellowship at Swedish Medical Center after completing the UCSF Family and Community Medicine residency in 2018. She practices full scope family medicine including outpatient, inpatient medicine, and labor and delivery where she cares for high risk OB patients, performs vacuum deliveries and cesarean sections with family medicine residents.
Nicole Person-Rennell, MD, MPH, FAAFP graduated from the UCSF FCM residency in 2017 and served as chief from 2017-2018. She works at the University of Arizona/Banner Health and is the medical director for the University of Arizona Mobile Health Program. This program provides care for patients without health insurance and other structural barriers to care, including a prenatal clinic.
September 6, 2024 - How UCSF partnered with the community for lasting impact on local Health Equity: Lessons, Challenges and Opportunities





(Starting top L)
Vanessa Bohm, MPH
Kent Woo, MPH
Christina Goette, MPH
Laura Schmidt, PhD, MSW, MPH
Roberto Ariel Vargas, MPH
UCSF’s Community Engagement resources were deployed for more than a decade to create a lasting impact toward Chronic Disease Equity. Via Collective Impact, we shaped health policy and the built environment, improved access to healthy foods in low-income communities, and created the largest source of funds for community-based organizations to engage in work that helped increase consumption of fruits and vegetables, reduce consumption of sugary drinks, and increase consumption of public drinking water, among other important things. Join us for a panel discussion about what we learned about Collective Impact and partnership along the way, and what opportunities lie ahead for community-university partnerships for health and UCSF.
Vanessa Bohm, MPH is the director of CARECEN SF’s Family Wellness and Health Promotion programs. She was born and raised in the San Francisco Bay Area by immigrant parents. She holds a B.A. in Psychology and an M.A. in Ethnic Studies. She has worked with Latinx and low-income families for more than twenty years, providing direct services and program management in the areas of family and youth support, health education and promotion. She has used her knowledge and experience to develop staff capacity, enhance program activities, and build partnerships that more effectively advocate, support, and improve the health and wellbeing of Latinx and low-income communities living in San Francisco. She has also dedicated much of her work to supporting the development of community health workers (promotoras de salud) to address health disparities in the Latinx community, such as chronic and diet-sensitive diseases and children’s oral health. Vanessa has also served as a health equity and policy advocate as a member of San Francisco’s Sugary Drinks Distributor Tax Advisory Committee and a member of the Chicano Latinx Indigena Health Equity Coalition.
Kent Woo, MPH has served the Asian American community for more than 35 years, the last 26 as the executive director of NICOS Chinese Health Coalition, a San Francisco-based public-private-community partnership of more than 30 health and human service organizations. A recipient of a Blue Cross of California Community Service Award (2003), Kent is a co-founder and first co-chair of the San Francisco A&PI Health Parity Coalition; a co-founder of the API Problem Gambling Task Force; a co-founder of the Asian and Pacific Islander Bay Area Health Council; a co-founder of the Chinatown Task Force on Children's Oral Health, a member of the Chinese Community Health Care Association Advisory Board; the California Department of Alcohol and Drug Program/ Office of Problem Gambling’s Advisory Committee; the Asian American Network for Cancer Awareness, Research and Training's Community Advisory Committee; the Chinese Community Cardiac Council. A native San Franciscan, he has served in several mayoral-appointed roles, including as a member of the San Francisco Department of Children, Youth and Families’ Citizens Advisory Committee and the San Francisco Census 2010 Complete Count Committee. He is formerly a Steering Committee member of the Building a Healthier San Francisco Collaborative and formerly a member of the Board of Directors of the Mental Health Association of San Francisco.
Christina Goette, MPH, since 1999, has worked for the San Francisco Department of Public Health, Community Health Equity and Promotion Branch and is currently Deputy Director, Wellness Programs. In 2006, she co-founded the Shape Up San Francisco Initiative. Her chronic disease prevention work focuses on policy and environmental prevention strategies to prevent and mitigate chronic disease health disparities and inequities related to nutrition and physical activity. In 2008, Christina led the initial Bay Area Regional Soda Free Summer campaign, and serves on local, state and national groups addressing sugary drinks. Christina worked with San Francisco policymakers to develop SF's 2014 and 2016 excise taxes on sugary drinks and volunteered on the campaigns. With the successful passage of the 2016 Sugary Drink Distributor Tax (SDDT), Christina's work has expanded to include staffing the Sugary Drink Distributor Tax Advisory Committee as well as managing over $3.5 million in SDDT revenue for community-based grants.
Laura A. Schmidt, PhD, MSW, MPH is a Professor of Health Policy in the School of Medicine at the University of California at San Francisco. She holds a joint appointment in the Philip R. Lee Institute for Health Policy Studies and the Department of Humanities and Social Sciences. She received her PhD training in sociology at UC Berkeley and while there, also completed doctoral coursework in public health. Dr. Schmidt seeks to understand how changing lifestyles are contributing to rising rates of chronic disease across the globe and what to do about it. Her work explores the growing pressures of globalizing economies, rising inequality, and the marketization of products that undermine our health. She works directly with policymakers to craft and implement evidence-based policies that reduce the consumption of ultra-processed foods and other commercial products that harm human and planetary health.
Roberto Ariel Vargas, MPH is Associate Director for the Center for Community Engagement and Senior Staff at the Community Engagement and RAGE Programs of UCSF’s Clinical and Translational Science Institute. Vargas has helped shape health policy and practice at the municipal and national levels on chronic disease prevention and cancer care, primarily by leveraging the expertise of UCSF scientists and community health advocates. Vargas served on the National Cancer Institute’s National Council of Research Advocates, the board of the Central American Resource Center (CARECEN) & co-chair of the SF Sugary Drinks Distributor Tax Advisory Committee & is currently on the board of the American Heart Association Bay Area & Instituto Familiar De La Raza. Prior to joining UCSF’s Department of Family and Community Medicine nearly 20 years ago, Vargas led community-based nonprofit organizations and school-based health and social service programs. As Director of the Real Alternatives Program Collaborative, Vargas began as a partner to UCSF on community-engaged research projects, and then as a community advisor to UCSF’s first community-university partnership program.
August 2, 2024 - Advancing Healthcare and Economic Development in Indian Country

Tyler Evans, MD, MS, MPH, AAHIVS, DTM&H, FIDSA Mark A. Echo Hawk, Esq.
This presentation explores the pressing issues of healthcare and economic development within Indigenous communities. Through a detailed examination of existing healthcare delivery systems and the historical context of Indigenous health services, this session sheds light on the disparities faced by American Indian and Alaska Native populations. We will discuss the critical role of Off Reservation 638 Tribal Health Centers in advancing quality care, accessibility, and economic growth. The presentation highlights innovative multidisciplinary models of care, including HIV street medicine, reentry services, and school-based health centers. With insights from an experienced MD and public health leader, and a Pawnee Tribe member and legal expert, the session underscores the importance of culturally intelligent programs, community engagement, and the social determinants of health. Attendees will gain a comprehensive understanding of the systemic changes needed to optimize healthcare delivery and promote economic development in Indian Country, starting with strategic public-private partnerships.
Tyler B. Evans, MD, MS, MPH, AAHIVS, DTM&H, FIDSA is the CEO and co-founder of Wellness Equity Alliance (WEA), a group dedicated to transforming public health care delivery to marginalized communities. During the COVID-19 response, Dr. Evans held several positions including the first chief medical officer (CMO) for NYC overseeing all COVID-19 operations in 2020, the CEO/CMO for Curative Medical Associates, and the deputy public health officer, chief of the COVID-19 vaccination branch at Marin County Health and Human Services Agency. He also served as one of the operational leads for the COVID-19 vaccination rollout with the Association of Bay Area Health Officers (ABAHO).
Dr. Evans has held other leadership roles focusing on homelessness, substance abuse, and migrant health, and led infectious disease divisions in various organizations across the US. As the national director of infectious disease for the AIDS Healthcare Foundation, he oversaw the implementation of hepatitis C programs, wellness centers, and behavioral health programs. He has also worked with large federally qualified health centers (FQHCs) in NYC and CA, and served indigenous communities with the Indian Health Service. Previously, he was the medical director for Alameda County’s Health Care for the Homeless, overseeing over a dozen street medicine programs.
With training in tropical medicine/infectious disease, internal medicine, preventive medicine/public health, and epidemiology, Dr. Evans has worked with vulnerable populations on international missions with organizations like Médecins Sans Frontières and Partners in Health. He co-founded the NYC Refugee and Asylee Health Coalition and a program in the eastern Democratic Republic of Congo to train primary care centers in mental health management for survivors of sexual and gender-based violence. He holds faculty appointments at USC and UCSF and has served on various boards and executive committees, including the HIV Medicine Association. Dr. Evans is the author of "Pandemics, Poverty, and Politics – Decoding the Social and Political Drivers of Pandemics from Plague to COVID-19."
Mark A. Echo Hawk, Esq. is an enrolled Member of the Pawnee Tribe and Co-Founder and Managing Principal of First Sovereign Health. Mark Echo Hawk leads a robust Indian law practice group. For over two decades, he has specialized in Indian law matters and championed Tribal interests. Mark represents Tribal governments on all governance matters, including Treaty rights, leasing and rights of way, taxation, 638 contracting, State and Federal government relations, tobacco regulation, health care, human resources, land and natural resource use, jurisdictional matters, contracts, code drafting and revision, grants, TERO, schools and education, Tribal courts, gaming, etc., and lobbying.
He focuses his practice on Tribal economic development, including Section 17 corporate charters and business organization, SBA 8(a) contracting, Tribal hotels and travel plaza development, mortgage and housing finance business, Tribal health insurance, and financial institution options. He also maintains an active practice representing businesses that work with Tribes or on Reservation lands. In addition to advocating for Tribal governments, Mark has also served as Tribal prosecutor and Tribal judge, and currently serves as the Chief Justice of the Pawnee Nation Supreme Court.
June 7, 2024 - Person-centered approaches to sexual and reproductive healthcare delivery through the lenses of health equity and racial justice


Diana Carvajal, MD, MPH Rachel Logan, PhD, MPH, CPH
This presentation delves into the critical issues of health equity and racial justice within sexual and reproductive healthcare. In this session, we examine the historical and structural roots of injustices in sexual and reproductive health, shedding light on longstanding inequities in care delivery. Through patient narratives and contemporary examples, we'll discuss how individuals with socially marginalized identities navigate the complexities of sexual and reproductive healthcare. With insights from a family physician and a public health researcher – drawing from data and lived experiences, we'll underscore the pressing need for systemic change, beginning with strategies for the clinical community.
Diana N. Carvajal, MD, MPH (she/her/ella) is an Associate Professor, a practicing family physician and a health services researcher in the Department of Family and Community Medicine at the University of Maryland School of Medicine (UMSOM). She is Director of Reproductive Health Education within the department’s residency program and also co-leads the department’s research division. She completed her residency at Columbia University Medical Center in NY, NY, her MPH at the Johns Hopkins Bloomberg School of Public Health, and her Primary Care Health Services Research fellowship at the University of Maryland School of Medicine. In her research, Dr. Carvajal focuses on addressing reproductive health inequities for the most disadvantaged communities and employs lenses of Reproductive Justice and Intersectionality to understand how clinicians can best support and communicate with their patients about important reproductive health decisions. In addition to her academic and clinical roles within the University of Maryland SOM, she is also the Director of Diversity, Equity, Inclusion and Strategic Planning for RHEDI based at the Montefiore Medical Center/Albert Einstein College of Medicine in the Bronx, NY. In this role, she leads the development and implementation of programs to diversify the reproductive health workforce in Family Medicine.
Rachel Logan, PhD, MPH, CPH, is a Research Specialist who completed a postdoctoral fellowship in the department and has a background in public health. Her work centers Black and other socially marginalized communities in strategies to improve sexual and reproductive health care experiences. She lives in Florida and is committed to realizing health equity and racial justice throughout the U.S., particularly in the Southeast.
May 3, 2024 - Family Medicine Physician Researchers: A critical component of an equitable and effective primary care infrastructure




Christine Dehlendorf, MD, MAS
Michael Potter, MD
Kevin Grumbach, MD
Anjana Sharma, MD, MAS
Hunter Holt, MD, MAS
Family medicine physicians are uniquely placed to understand what research should be done to improve the ability of our health care system to provide equitable, patient-centered primary care. However, the culture of family medicine does not always recognize or embrace this potential, at least in part due to the perception that research is inherently disconnected from the immediate needs of the communities we serve. In this session, five family medicine physicians who conduct research on a range of topics and using a range of methodologies will discuss their paths to becoming clinician researchers, and how their identity as a family physician interrelates with and informs their identity as a researcher. They will further reflect on the relationship of their research, and of research in general, to our departmental mission to advance health equity.
Christine Dehlendorf, MD, MAS, is a Professor and Vice Chair for Research in the Department of Family and Community Medicine at the University of California, San Francisco, with additional appointments in the Departments of Obstetrics, Gynecology and Reproductive Sciences and Epidemiology and Biostatistics. She founded and directs the Person-Centered Reproductive Health Program, which aims to advance reproductive autonomy and well-being by conducting research and designing programs that center people’s experiences and preferences for sexual and reproductive health and health care, guided by an attention to the intersecting oppressions and structural injustices that impact people’s lives and health. She also provides primary care and reproductive health care at the Family Health Center at San Francisco General Hospital and Planned Parenthood.
Michael Potter, MD is a graduate of the family medicine residency program at UCSF’s San Francisco General Hospital, where he also served as chief resident. He has been a professor in UCSF’s department of family and community medicine for nearly 30 years. During the course of his career he has split his time in variable proportions between clinical care, teaching, and practice-based research. His research has always been informed by the experiences and insights of practicing family physicians caring for diverse communities and patient needs with limited resources. Findings from several of his research studies have been disseminated and incorporated into common clinical practice nationally. He currently directs several programs within UCSF’s Clinical and Translational Science Institute, including its Research Infrastructure Network, Collaborative Research Network, and Team Science Program.
Kevin Grumbach, MD is Professor of Family and Community Medicine at the University of California, San Francisco. He served as Chair of the UCSF Department of Family and Community Medicine from 2003-2022. He is a Founding Director of the UCSF Center for Excellence in Primary Care and Director of the Community Engagement Program for the UCSF Clinical and Translational Science Institute. Throughout his career he has wrestled with translating his research and scholarship on the primary care workforce, innovations in primary care, racial and ethnic diversity in the health professions, and community health improvement and health equity into changes in policy and practice. Dr. Grumbach has been an advisor to Congressional Committees and government agencies on primary care and health reform and a member of the National Advisory Council for the Agency for Healthcare Research and Quality, and currently serves on the California Health Workforce Education and Training Council.
Anjana Sharma, MD, MAS, is Associate Professor of Family & Community Medicine. She practices at the Family Health Center at San Francisco General Hospital. Her research focus is patient and community engagement in primary care. This includes implementing and assessing patient advisory councils, community-engaged research on telehealth, and involving patients and community in the FCM residency.
Hunter Holt, MD, MAS is a board-certified family medicine physician and assistant professor in the University of Illinois, Chicago Department of Family and Community Medicine. Dr. Holt is focused on researching and implementing solutions that improve patient experiences and health outcomes related to reproductive health and cervical cancer prevention. In medical school, at Rush University, Dr. Holt traveled to China as a NIH Fogarty Global Health Fellow to research cervical cancer prevention in China. Working with the Cancer Institute of China, Dr. Holt investigated cervical cancer screening in Chinese migrant workers and post-menopausal Chinese women. As a family medicine resident at the University of Illinois, Chicago, Dr. Holt was a part of the Global Health Track working in Senegal to implement sustainable solutions for cervical cancer prevention in rural Senegal. As a Primary Care Research Fellow at UCSF, Dr. Holt completed his master’s degree in Clinical and Epidemiological Research and worked to understand the reasons behind disparities in cervical cancer incidence and mortality. Currently Dr. Holt is working to finding solutions to reduce these cervical cancer disparities and promote health equity.
April 5, 2024 - The Changing Landscape of Primary Care: a Canadian perspective

Danyaal Raza, MD
In this presentation, Dr. Raza will (1) Provide a brief overview of the Canadian health care system, (2) outline how primary care and family medicine fit in, and (3) explore the contemporary crisis and opportunities for reform.
Danyaal Raza is a family physician with Unity Health Toronto’s St. Michael’s Hospital, and Assistant Professor with the University of Toronto’s Department of Family & Community Medicine. He is the founding physician lead of the Sumac Creek Health Centre in Toronto’s Regent Park, the largest social/public housing community in Canada, and a member of the Decent Work & Health Network. Dr. Raza has also served as Chair of Canadian Doctors for Medicare, is a Fellow of the Broadbent Institute, and in 2021 was named to The Medical Post’s ‘Power List’ as an influential physician voice in Canadian health policy.
March 1, 2024 - Community Grand Rounds: Equitable Relationships for Equitable Health Outcomes



Shavonne Allen Sam Dennison Freddy Martin Monica Hahn, MD
In this Grand Rounds presentation, we are putting community voices front and center. Residents of the Tenderloin (San Francisco’s most diverse neighborhood) and Dr. Monica Hahn (FCM) will be in dialogue with each other and with you, discussing strategies for creating effective, supportive collaborations for institutional and structural change at UCSF. We began this work in 2021, amid the chaos of COVID and discovered in the process what it looks like to mutually honor the experiences of those struggling to access care and those juggling inequitable resources and burnout as they provided care. We will tell you the history of this project, how it supports our work as community and healthcare advocates, and how you can find your place in similar communities of change agents.
Shavonne Allen, Skywatchers Ensemble, San Francisco Artist and Resident, is a community leader whose creative talents bring light to the needs of the community and uplifts the talents of all.
Sam Dennison, Faithful Fools, Tenderloin Resident, is a community advocate who challenges UCSF to deepen community partnerships with unlikely allies for deep institutional change.
Freddy Martin, Congregational Life & Community Engagement Manager Glide Memorial Church, Skywatcher, whose depth of commitment brings people together and knits community threads into vibrant patterns.
Monica Hahn, MD, MPH, MA, AAHIVS, Associate Clinical Professor at UCSF in the Department of Family & Community Medicine and OBGYN, is a valued community collaborator and liaison between UCSF and community residents who opens UCSF doors to otherwise unheard community voices.
February 2, 2024 - Preparing the Next Generation of Leaders and Change Agents

Katherine Mathews, MD, MPH, MBA
In this Grand Rounds presentation, Dr. Mathews will discuss strategies for training medical students to be leaders and change agents in medicine and society at large. Many medical students bring passion to our profession and are often distressed to learn about the entrenched structural inequities within the US health care system. This combination of passion and distress can lead students to jump to solutions that have the potential to do more harm than good. By focusing on self-awareness, moral humility, perspective taking, teamwork, and cultivating a "lifelong learner" mindset, Dr. Mathews prepares students for leadership as a long-term endeavor that is best done in partnership with others. She will review both opportunities and challenges with this approach.
Katherine Mathews, MD, MPH, MBA, is an Ob/gyn physician with a background in international work, healthcare administration, and public health. She has lived and worked in St. Louis, Missouri, for over 25 years and has been engaged in many regional initiatives to improve access to quality care for low-income communities. She currently serves as the Associate Dean of Health Systems Science at Saint Louis University School of Medicine where she teaches leadership and oversees many community focused initiatives.
December 1, 2023 - Expanding Self-Injectable Contraceptives in the US from a Person-Centered Perspective

Jennifer Karlin, MD, PhD
In this Grand Rounds presentation, Dr. Karlin will focus on her research in expanding injectable contraceptives in the US for self-injection. She will trace three steps of a research program thus far—starting with an implementation project at the Family Health Center during the COVID-19 pandemic, to qualitative interviews with patients in San Francisco and Washington State, to a nation-wide survey and interviews of interprofessional health care providers about barriers and facilitators to expansion of the contraceptive. Tracing these three arms of this research program so far and discussing next steps, Dr. Karlin will use this example of expanding self-injectable contraceptives to illustrate how research can remain centered on equity, sustain a person-centered lens, and develop more formal research plans from an emergent need.
Dr. Karlin, MD, PhD, is a board-certified family physician and fellowship-trained family planning specialist who completed her residency and fellowship in this department and currently is on faculty at UC Davis. She focuses on expanding and supporting reproductive and sexual health through primary care. Trained as an anthropologist and historian of medicine, her research addresses how we can alter health care relationships and systems to encourage patient empowerment, autonomy, and equity. Additionally, Dr. Karlin is committed to medical and resident education that encourages physicians-in-training to approach their practices from an historical, trauma-informed, and self-reflexive perspective to improve quality of care and decrease additional trauma caused by the medical system.
November 3, 2023 - Health Services and Outcomes Research to Support Quintuple Aim in Primary Care

Tapan Mehta, PhD, MSEE
This presentation will describe use of pragmatic study designs and artificial intelligence/machine learning to develop sustainable and scalable programs to improve population health outcomes and address health equity. Studies illustrating use of these designs will be presented. The relevance of these techniques to support a learning health system approach for primary care will be shared.
Tapan Mehta, PhD, MSEE, is a health services researcher with training in biostatistics and engineering. He currently serves as a tenured Professor and Vice Chair for Research at University of Alabama at Birmingham’s Department of Family and Community Medicine with a secondary appointment in the Department of Health Services Administration. His independent research interests are in health services and outcomes research related to disabilities and cardiometabolic conditions with a focus on knowledge generation in pragmatic settings, and strategies in translating knowledge that can influence practice and policy. He is an MPI of two NIH-funded optimization studies focused on developing sustainable diabetes management programs to support health equity. He also leads the data coordinating center for the CDC-funded National Center on Health, Physical Activity and Disability with an objective of health equity for people with disabilities and co-directs the NIH-funded Nutrition Obesity Research Center’s Behavioral Science and Analytics. He has published over eighty peer-reviewed articles, and authored/co-authored in journals such as JAMA, New England Journal of Medicine, Obesity, Nature Genetics, and American Journal of Physical Medicine and Rehabilitation.
October 6, 2023 - Expanding on Alcohol Harm Reduction: The San Francisco Department of Public Health Managed Alcohol Program



Alice Moughamian, RN and CNS Bryce Bridge, LMFT Tanya Majumder, MD MS
The San Francisco Department of Public Health's Managed Alcohol Program (MAP) started in 2020 as a COVID I&Q response for people who drink alcohol but has become a permanent part of the city's harm reduction services. During our presentation, we will discuss how our MAP began, define the scope and purpose of MAPs, describe the different MAP care models in the literature, and identify key ethical issues at play in alcohol harm reduction work.
Alice Moughamian, RN serves as Nurse Manager of the Managed Alcohol Program and the San Francisco Sobering Center for the San Francisco Department of Public Health. In addition to this role, she was Nurse Manager and Program Director of the Medical Respite Program as well as nursing services in permanent supportive housing before devoting full time to Managed Alcohol and Sobering. She completed the CHCF Healthcare Leadership Fellowship in 2020. Alice has also served as Chair of the National Healthcare for the Homeless Council’s Respite Care Providers Network and helped develop national standards for Medical Respite care. She worked as a floor nurse at UCSF Medical Center for 4 years and did her clinical studies for her Masters degree at Zuckerberg San Francisco General Hospital’s Positive Health Program. Alice served as a Peace Corps volunteer in the Dominican Republic for 3 years between college and nursing school. When not working, Alice’s greatest joy is going on new adventures and spending time with her husband and two children.
Bryce Bridge, LMFT is a clinical supervisor for Sobering Center Case Management, a low-barrier, intensive-case management program for people who use alcohol. Bryce obtained his master's degree in clinical psychology from San Francisco State University and is a Licensed Marriage and Family Therapist. Bryce has worked in community mental health and substance treatment with marginalized populations throughout the past decade and has been employed at UCSF Citywide Sobering Center Case Management since 2019.
Tanya Majumder, MD is the Lead Physician of the Managed Alcohol Program and the Sobering Center and is also a primary care physician with Street Medicine, Shelter Health, and Urgent Care. She completed medical school and her master's in health and medical sciences at the Joint Medical Program between Berkeley and UCSF before attending residency in Internal Medicine-Primary Care at the Yale Primary Care program. She has greatly enjoyed being part of the Whole Person Integrated Care team for the past 4 years.
September 1, 2023 - Aging and End of Life Care in an Incarcerated Setting

Michele DiTomas, MD, MS
Decades of harsh sentencing laws have resulted in over 200,000 people in the Unites States currently serving life sentences with a disproportionate impact on people of color. In California, despite an overall decline in the numbers behind bars in the last decade, the number of people age 55 and older has nearly doubled. Studies have shown that the chronic disease burden and degree of functional impairment of incarcerated people is similar to those 10-15 years older in the community as more and more older adults are facing the prospect of aging, coping with serious illness and dying in prison. How do we, as a society and as clinician advocates better meet the needs of this aging population pre-sentencing, during incarceration and upon reentry?
Michele DiTomas, MD, MS is currently the Chief Medical Executive over the Palliative Care Initiative with the California Correctional Healthcare Services, which strives to improve whole person care for those struggling with the challenges of serious illness and aging behind bars. Since 2007, she has served as Chief Physician and Hospice Medical Director at the California Medical Facility, which provides end of life care to men incarcerated in the California Department of Corrections. She earned her MD from the UCSF/UC Berkeley Joint Medical Program and completed her residency at the UCSF Department of Family and Community Medicine.
As Hospice Medical Director she works with the hospice team to create an environment where patients can live their final days with dignity, respect and comfort despite their incarceration. The hospice team supports the patients and their families in achieving compassionate release and, when this is not possible, provides a setting where they are able to have meaningful visits and often find reconciliation and closure at the end of life.

Maddie Deutsch, MD, MPH
Trans and Gender Diverse People need access to quality healthcare. This "Gender Affirming Care" can include medical or surgical care to align one's body with their identified gender, as well as access to a full scope of medical care that is respectful and culturally grounded, and acknowledges gender identities as valid. Recent political developments have added an additional layer of complexity to the barriers to care and disparities faced by this vulnerable population. In this talk, Dr. Deutsch will review current evidence in selected areas of gender affirming care for children, adolescents, and adults of all ages.
Maddie Deutsch, MD, MPH is a Professor of Clinical Family & Community Medicine at UCSF, and the founding Medical Director for the UCSF Gender Affirming Health Program, a multidisciplinary group of medicine, surgical, and behavioral health providers for trans and gender expansive adults at UCSF Health. She is a Co-Director for the UCSF School of Medicine Differences Matter Initiative, and a DEIB Co-Lead for UCSF Health. Dr. Deutsch has authored or co-authored more than 50 peer reviewed journal articles in the field of sexual and gender minority health, and was a co-author, and Primary Care Chapter Lead, for the recently released WPATH Standards of Care, 8th Version. She is the current President of the US Professional Association for Transgender Health.

Kevin Fiscella, MD, MPH
Concepts matter. There is a current political struggle in the US over the meanings of "race," "racism," and "wokeness." In this presentation," I argue that defining "health" is a radical idea. The meaning of health has profound implications for how we organize research, healthcare, and ultimately society. For this reason, our nation has avoided defining health. This definitional void yields a default disease-based biomedical definition of health. The consequences of this default definition are profound: 1) enabling research and healthcare funding that supports the biomedical-industrial-healthcare complex; 2) obscuring deeper meanings of health equity; 3) trivialization of social determinants of health 4) marginalization of primary care; 5) contributing to unprecedented declines in national health, wellbeing; and 6) perpetuation of gross inequities in health. The concept of health has profound implications for what it means to be human, to care for self and others, and for the social conditions that enable people to optimize their full health potential. We need a national dialogue on the meaning of health and critically how to enable it through research, healthcare, and societal change.
Kevin is a tenured professor in the Department of Family Medicine at the University of Rochester School of Medicine. He is co-director of the department research division and co-director of the equity-focused dissemination and implementation core within the University of Rochester Clinical and Transnational Science Institute. He is worked as a family physician in FQHCs caring for multigenerational families, including people living with HIV and substance use disorder, for 40 years. He is a health services researcher whose research career has addressed health and healthcare equity. His current research and mentoring involve the application of implementation science to promote health equity within health care and the community. Kevin is currently leading a scoping review for AcademyHealth on equity and value in US healthcare and a NASEM-commissioned review of trends in racial and ethnic inequities in healthcare access and quality in the US.
May 5, 2023 - The Present Illness: American Health Care and Its Intractable Afflictions
Martin Shapiro, MD, PhD, MPH
Drawing on the analyses in his recent book, The Present Illness: American Health Care and Its Afflictions, Dr. Shapiro will explore the reasons why it has been so difficult to solve the many problems in American health care. He identifies three underlying phenomena that shape the behavior of physicians and their organizations, medical schools and their faculty, hospitals and health systems, other corporations in the health sector, scientists and their sponsors, and also patients and the public. These are the commodification of health care and health by all the groups of participants; the consciousness of the actors—their attitudes, values, expectations, interests, and perceived needs; and the communication and the structure of the relationships across these groups, which tend to reinforce the worst tendencies in all groups. He will discuss a range of steps that can be taken to address these many problems, but that meaningful reform will need to be broad and deep.
Dr. Martin Shapiro obtained his medical degree from McGill University and a PhD in history and Master’s in Public Health from UCLA. He is Professor of Medicine at Weill Cornell and Distinguished Professor Emeritus of Medicine and Public Health at UCLA. Prior to coming to Cornell, he spent many years at UCLA, where he was chief of the Division of General Internal Medicine and Health Services Research for 25 years. He is a general internist who has practiced both inpatient and outpatient GIM. He also is a health services researcher who has studied accessibility of care and health disparities, scientific misconduct, pharmaceutical advertising, and scientific authorship, among other topics. He led a major national study of care for HIV disease. He is also interested in such conditions as hypertension and hepatitis C, in empowering communities in relation to the research enterprise, and in trying to improve health and health care for those most in need. He is an elected member of the American Society of Clinical Investigation and of the Association of American Physicians and is a past president of the Society of General Internal Medicine. He enjoys mentoring students, residents, fellows and junior faculty members. His new book, The Present Illness: American Health Care and Its Afflictions, has just been published by Johns Hopkins University Press.
April 7, 2023 - Demoralization in Medicine with a focus on Strategies and Solutions

Megan Mahoney, MD
Changes in the health care system have altered the nature of primary care clinician’s interactions with patients and our sense of empowerment to improve the practice environment. Profound health disparities have caused disillusionment and dwindling faith in the systems for which we work. Strategies and solutions lie in the fact that we are internally motivated when we believe in what we are doing and feel part of a community. The objective of this presentation is to review the evolution of demoralization in medicine and discuss evidence for coalition-building to drive change and restore wellbeing.
Dr. Megan Mahoney is the Hellman Endowed Professor and Chair in the UCSF Department of Family and Community Medicine. Throughout her career, Dr. Mahoney has built and led sustainable initiatives in provider engagement, quality improvement, and DEI for health care organizations. Her research has focused on the impact of primary care team cohesion on burnout, and the influence of diversity and inclusion on individual and team wellbeing. She has presented on team wellness as a keynote speaker at national and international meetings, and served as long-term faculty for the national Chief Wellness Officer Course – an executive program for physician well-being leaders. Dr. Mahoney earned her B.A in Molecular and Cellular Biology at the University of California Berkeley and her M.D. at the University of California San Francisco. She completed the UCSF Family Medicine Residency Program at San Francisco General Hospital.
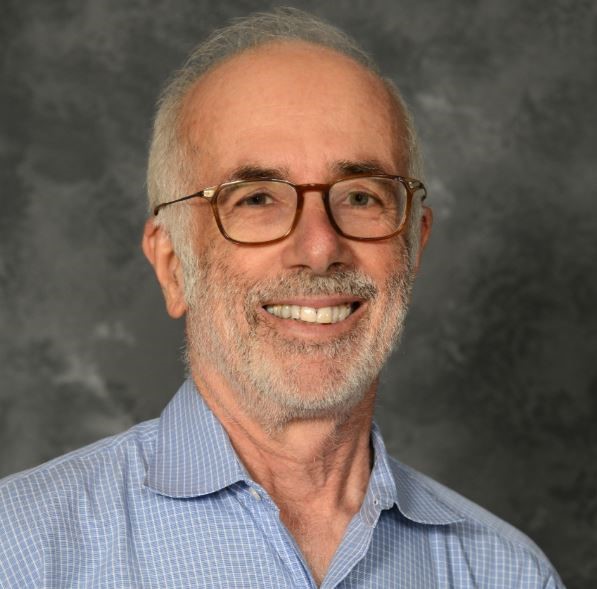
March 3, 2023 - What is Medicine For? - Reflections from On Medicine as Colonialism

Michael Fine, MD
What is Medicine For? - Reflections from On Medicine as Colonialism uses On Medicine As Colonialism as a point of departure to discuss evidence-based ways in which medicine and healthcare can be effective at improving population health, as we strengthen and bring resilience to communities. Dr. Fine encourages residents to keep their eyes on the prizes of population health and community resilience and to listen to patients and communities, so that physicians in training aren't overwhelmed by the demands of healthcare bureaucrats and profiteers.
Michael Fine, MD is an award-winning author, community organizer, public health expert/leader, and family physician. Dr. Fine is the author of On Medicine As Colonialism (PM Press, 2023), which explores the way medicine and health care have been used by health care profiteers to co-opt the state’s regulatory power, Medicare, and Medicaid and extract resources from communities and upend democracy in the U.S.; Health Care Revolt, an expose, manifesto and playbook that exposes the failures of the healthcare market to deliver health and plans a movement to build the healthcare system the US needs (PM Press, 2018); Abundance, a novel about two young Americans caught up in the Liberian civil wars of 1998-2003 (PM Press, April 2019); The Bull and Other Stories (Stillwater River Press, 2020) ; and Rhode Island Stories (Stillwater River Press, 2021). He is the coauthor, with James W. Peters, of The Nature of Health (Radcliffe, 2007), a study of healthcare services, human rights, society, technology, and industry; and The Zero Calorie Diet (Red House Press, 2010), a look at the culture of excess through the lens of fasting. The Bull and Other Stories was the 2021 IPNE Literary Fiction Book of the Year.
Dr. Fine serves as Chief Health Strategist for the City of Central Falls Rhode Island. Dr. Fine served in the Cabinet of Governor Lincoln Chafee as Director of the Rhode Island Department of Health 2011-2015, overseeing a broad range of public health programs and services, 450 public health professionals and managing a budget of $110 million a year.
February 3, 2023 - San Francisco's Approach to Improving Behavioral Health Services

Hillary Kunins, MD, MPH, MS
As we navigate multiple, intersecting public health crises, including the COVID-19 pandemic, systemic racism, homelessness, and the opioid/fentanyl overdose epidemic, there is unprecedented need for mental health and substance use care in the City. Dr. Kunins will share how the San Francisco Department of Public Health is growing and transforming behavioral health services to expand access to timely, equitable, and well-coordinated care.
Dr. Hillary Kunins is the Director of Behavioral Health Services and Mental Health San Francisco at the San Francisco Department of Public Health (SFDPH). In 2021, she joined SFDPH from the New York City Department of Health and Mental Hygiene (DOHMH) where she served as the Executive Deputy Commissioner of Mental Hygiene from 2019 to 2021 and as the Assistant Commissioner for the Bureau of Alcohol and Drug Use from 2012 to 2019.
At DOHMH, Dr. Kunins led the reimagining of New York City's public health approach to substance use and served as the DOHMH lead for Mayor Bill de Blasio’s $60 million HealingNYC initiative to address the overdose epidemic. She has dedicated her career to creating health equity through science-based public health and healthcare programs and policy for people with behavioral health concerns, including substance use disorders and serious mental illness.
Dr. Kunins received her MD and MPH from Columbia University and her MS in Clinical Research from Einstein College of Medicine. She completed her primary care-internal medicine residency and chief residency at Montefiore/Einstein. Dr. Kunins is a Fellow of the American College of Physicians and of the American Society of Addiction Medicine.
December 2, 2022 - An Equity First Paradigm for Health Care: Hard Earned Lessons from the UCSF Health Response to COVID



Pilar Collins, MPH, MSW, PMP Tasha Toliver, MSHE Kevin Grumbach, MD
The UCSF Health COVID Equity Work Group was formed in November 2020 to address racial-ethnic inequities in COVID-19 among UCSF Health patients, UCSF employees, and the San Francisco community. Members of the COVID Equity Work Group will describe the multifaceted interventions implemented to promote equity in COVID vaccination. An evaluation of these efforts informed development of a new framework—an Equity First paradigm—that shaped ensuing UCSF Health equity interventions for COVID test-to-treat strategies and MPX vaccination. The presentation will highlight both the progress achieved and the ongoing challenges in moving a large health care institution to make Equity First a standard operating procedure.
Pilar Collins is a Senior Organizational Consultant in the Health Equity Division, Department of Quality and Patient Safety, at UCSF Health, and co-chair of the COVID Equity Work Group. The Health Equity division serves as the health system’s strategic and operational engine to advance health care equity. Pilar has a keen focus on leading UCSF Health to define and operationalize an Equity First strategic vision and framework. Prior to her current position, Pilar worked in Information Technology at UCSF Health, where she was the Manager leading UCSF Clinical Systems Customer Engagement applications team supporting the new technologies at Mission Bay Hospital and prior to that was the Information Technology Program Manager on the Mission Bay Hospitals project construction team, leading multiple infrastructure and applications teams. She has both a Master’s Degree in Public Health and Master’s Degree in Social Work from UC Berkeley and is a certified Project Management Professional.
Tasha Toliver is the manager for UCSF Health’s Population Health Outreach team which focuses on closing care gaps. Prior to this position she was the operations manager for UCSF’s COVID hotline which was created at the beginning of 2020 in response to the pandemic, and won a UCSF Health Team PRIDE award in 2021. She originally joined the Office of Population Health in 2014 as a Health Care Navigator with the Care Support Program. This team was awarded a Team PRIDE award in 2018. She holds a Master’s Degree in Health Education from Kaplan University. Tasha has a passion for Diversity, Equity, and Inclusion work and has presented at UCSF’s Town Hall on Health Equity interventions.
Kevin Grumbach is Professor of Family and Community Medicine at UCSF. He served as Chair of the UCSF Department of Family and Community Medicine from 2003-2022, and as Vice President for Population Health for UCSF Health from 2015-2018. He is co-chair of the Health Equity Work Group at UCSF Health. He is a Founding Director of the UCSF Center for Excellence in Primary Care and Director of the Community Engagement Program for the UCSF Clinical and Translational Science Institute. He cares for patients at the Family Health Center at San Francisco General Hospital and the Lakeshore Family Medicine Center at UCSF Health.
November 4, 2022 - Safety for All and Care without Criminalization: A DPH Must Divest Intro to Patient Rights





Ana Delgado, Ji Seon Song, Nida Bajwa, Norman Archer, Jake Sonnenberg, Kelley Butler
Over the last two years DPH Must Divest has organized at SFDPH to abolish contacts with the San Francisco Sheriff’s Department, build-up non-policing crisis responses, and transform the culture of our hospitals and clinics. SFDPH is in the violent minority as one of the <1% of systems nationwide dependent on law enforcement alone to provide security. We know that policing in the hospital is a racial justice issue, with 70% of use of force incidents being against Black patients and visitors in the ED in 2019, despite representing only 24% of the patient population. In this Grand Rounds presentation, we will give a framework for thinking about abolition and the history of our campaign to get the Sheriffs out of our hospitals and clinics. We will then introduce Know Your Rights materials regarding policing in the hospital, presented by a law professor and law school graduate, and ground these protections in a conversation between two FCM Residents. Finally, we will offer further resources to interrupt criminalization and get involved with our campaign.
Ana Delgado, MS, RN, CNM is a Clinical Professor in the Department of OBGYN, SFGH Division. Ana splits her time between clinical practice and administration, teaching, and community-based advocacy. Ana is active both regionally and nationally in efforts to diversify the midwifery workforce, support physiologic birth, and participates in community-based efforts to support and care for people throughout the reproductive life cycle. Ana sees abolition as a key part of ensuring that families can thrive.
Ji Seon Song is a professor of law whose teaching and research focuses on criminal law, criminal procedure, and policing. Prof. Song’s scholarship examines the deployment of policing authority and corresponding effects on racial minority and other marginalized groups. Her research informs interventions that address race- and class-based disparities in policing practices. Prof. Song’s scholarship draws on her years of practice experience. Previously, Prof. Song represented youth and adults as a Deputy Public Defender at the Contra Costa County Office of the Public Defender and as a Prettyman Fellow at the Georgetown University Law Center. She also worked as a senior policy advocate for the National Juvenile Defender Center. Prof. Song joins UCI Law from Stanford Law School, where she was a Thomas C. Grey Fellow and Lecturer in Law while developing an extensive research project on policing in hospitals.
As part of her research on policing in hospitals, Prof. Song regularly conducts trainings and provides consultation for medical providers on the intersection of medical care and policing. Prof. Song is also a well-known advocate for local, regional, and national juvenile justice reform. She currently serves on the Executive Board of the Pacific Juvenile Defender. Prof. Song clerked for the late Honorable Deborah A. Batts of the Southern District of New York.
Prof. Song earned a B.A in East Asian Languages and Cultures with a minor in Music from Columbia College, Columbia University, a J.D. from Columbia University School of Law, and an LL.M. from Georgetown University Law Center.
Nida Bajwa is a second-year UCSF resident in family medicine. She graduated from Northwestern University with a degree in journalism and global health studies. In medical school she was involved in anti-deportation and anti-racist work.
Norman Archer is a third-year medical student at UCSF. He completed his undergraduate degree at the University of North Carolina, Chapel Hill, where he studied public health, nutrition, and medical anthropology. He previously worked in advocacy, policy, and research at Housing Works in New York City.
Jake Sonnenberg is a third-year medical student at the University of California, San Francisco. He completed his undergraduate degree at Stanford University, where he studied Human Biology and History, and he holds a J.D. from Stanford Law School. He previously worked in health and social policy and remains involved in advocacy and research to repair the policy failures that drive healthcare injustice.
Kelley Butler is a resident physician in family medicine at the Zuckerberg San Francisco General Hospital in partnership with the University of California San Francisco. She graduated from the University of California, Irvine School of Medicine. Hailing from Los Angeles, Kelley has committed herself to serving marginalized communities. She is an active member in various causes dedicated to students and professionals of color, people suffering from substance use disorder and addiction, and those without access to basic needs. On her medical campus and now in residency, Kelley is known for her work in social justice, health advocacy, health policy and initiatives targeted for minoritized trainees. She currently holds leadership positions within the Council of Interns and Residents, a union for residents and fellows, and Doctors for America, a national organization committed to progressive causes and physician advocacy.
Kelley completed her Masters of Public Health in Health Policy at the Harvard TH Chan School of Public Health. There, she lead organizing efforts in juvenile justice reform and prison divestment, presented research on substance use and addiction treatment, completed a fellowship in Equity, Diversity and Inclusion, increased civic engagement on campus through the Harvard Votes Campaign and oversaw a workshop series on Imposter Syndrome. Following her masters studies, she went on to serve rural and frontier communities in Oregon as an Opioid Response Program Associate for Greater Oregon Behavioral Health Inc.
Kelley graduated from Howard University in 2015 with a passion for serving communities without access to health insurance, quality healthcare or education. As such, she’s dedicated herself to educating and serving both local and international communities in need. She’s traveled to Panama, Kenya and Angola on medical missions thus far and looks forward to continuing to be of service to all mankind.
October 7, 2022 - From Eggshells to Action: Preparing to Address Microaggressions Targeting Learners

Meghan O'Brien, MD, MBE
Microaggressions, or dignity violations, occur frequently in the clinical learning environment. When patient microaggressions target learners and supervisors fail to respond, the harm caused is compounded by faculty inaction. Informed by her team's research on student and supervisor experience with patient microaggressions targeting medical students, Dr. O'Brien will discuss a framework for microaggression response and highlight key attributes of skilled responders to help support supervisor bystander action when patients microaggress learners.
Meghan O'Brien, MD, MBE, is an Assistant Professor at UCSF, and a hospital-based general internist at San Francisco General Hospital where she leverages her training in primary care, humanities, and bioethics to provide dignity-driven, whole-person care. She completed her undergraduate degree in American Studies at Brown University, her medical degree and Masters of Bioethics at the University of Pennsylvania, and her Internal Medicine residency at UCSF’s Primary Care track before joining the ZSFG’s Division of Hospital Medicine. Dr. O'Brien is a member of UCSFs Academy of Medical Educators, and a Bridges Coach for the SJV-PRIME program. She splits her non-clinical time between medical education, advancing diversity, equity, and inclusion in medical education, and addiction medicine.
September 2, 2022 - Moving from Intention to Action on Health Equity

Ayanna Bennett, MD, MS, FAAP
In our post-George Floyd world, many organizations and individuals have committed to eliminate health inequity. However, many seem to focus on generating understanding and goodwill rather than concrete change. Dr. Bennett will discuss a framework for health equity implementation that the Office of Health Equity is developing at San Francisco Department of Public Health. This is an evolving framework, but the best practices around health equity are all evolving and this framework is offered as one potential approach.
Dr. Ayanna Bennett is the Chief Health Equity Officer and Director of the Office of Health Equity at the San Francisco Department of Public Health. Dr. Bennett is a pediatrician, trained for her MD at UCSF and in the UCB-UCSF Joint Medical Program for a Master’s degree. In 2004, Dr. Bennett co-founded a non-profit in the San Francisco Bayview Hunters Point neighborhood called the 3rd Street Youth Center and Clinic, which is thriving today. Dr. Bennett led 3rd St as its Medical Director and then Executive Director for 12 years, while also working as a practicing pediatrician in the East Bay. Dr. Bennett transitioned fully to the Health Department in 2015, taking several leadership positions before establishing the Office of Health Equity in 2019. OHE focuses 4 areas, creating a diverse staff with health equity competency, reducing health disparities, supporting a culture of accountability and authentic community engagement.
June 3, 2022 - The Political Determinants of Health: Advocating for Equitable Health Outcomes

Daniel Dawes, J.D.
Today, it is commonly understood that health outcomes are influenced by more than genetics and behavior. In fact, many health problems can be firmly linked to a political action or inaction (Dawes, 2020). Our political system has not always valued each group equally much less realized the long-term implications of policies on the health of its citizenry. Conditions in the places where people live, learn, work, and play, can have a wide range effect of health risks and outcomes (CDC, 2021).
However, the real instigators or drivers of these unjust and inequitable outcomes, are the Political Determinants of Health (PDoH) which involve the systematic process of structuring relationships, distributing resources and administering power, operating simultaneously in ways that mutually reinforce or influence one another to shape opportunities that either advance health equity or exacerbate health inequities (Dawes, 2020). These determinants and drivers are what have given way to racism and health inequity in America which remain to be addressed. Before we can begin to look beyond to a more equitable America, we must first understand the foundational nature of the political determinants of health’s and their systemic influence and structural concretization i.e. the “isms” plaguing the United States. Equally paramount, is to offer novel solutions including policies, that will forge a path towards recovery and ultimately, advancing health equity for all.
Daniel E. Dawes, J.D., is a widely respected healthcare and public health leader, health policy expert, educator, and researcher who serves as executive director of the Satcher Health Leadership Institute at Morehouse School of Medicine and a professor of health law, policy and management. A trailblazer and nationally respected voice in the health equity movement, his scholarship and leadership, particularly the innovative political determinants of health framework that he pioneered, have resulted in increased policies and laws prioritizing health equity. By tackling upstream determinants of health, he has ventured into such uncharted territory as the intersection between equity and the social and political determinants of health to change the course of domestic and global policies for the better.
His groundbreaking works, 150 Years of ObamaCare, which document the health equity movement in America and elevates the health equity-focused provisions of the Affordable Care Act that he led in negotiations and formulation, and The Political Determinants of Health, which provides an in-depth lens on the root causes of inequities, both published by Johns Hopkins Press are now nationally and internationally recognized and used as top health policy books. His passion for addressing health inequities is exemplified in his unyielding commitment to building collaboratives, including the HHS grant-funded National COVID-19 Resiliency Network and the Health Equity Leadership & Exchange Network, both exist to leverage evidence-based research and develop actionable solutions to advance health equity.
Professor Dawes’ work focuses on health reform, health equity, mental/behavioral health inequities, social and political determinants of health, poverty, and health system transformation. His work bridges research, technology, healthcare, population health and public health – the translation of research discoveries into all communities, including under-resourced, vulnerable, and marginalized communities. Professor Dawes brings a forward-thinking, inclusive, and multidisciplinary approach to address issues impacting diverse populations in urban and rural communities in our progressively complex health system, including a national study examining the health and economic impact of mental health inequities in the United States and a major research project which created the nation’s first health equity tracker. Among his many achievements, he was an instrumental figure in developing and negotiating the Mental Health Parity Act, the Genetic Information Nondiscrimination Act, the Americans with Disabilities Act Amendments Act, and an architect of the Affordable Care Act’s health equity-focused provisions, among other landmark federal policies.
Professor Dawes is an elected member of the National Academy of Medicine and an elected fellow of the New York Academy of Medicine. He serves as an advisor to The White House COVID-19 Health Equity Task Force and an appointed member of the CDC’s Advisory Committee to the Director.
May 6, 2022 - "Anti-coercion Ethics and the Avoidance of Medical Harm: A Case-based Discussion"



A discussion about the impact of race, social identity, intersectionality and positionality on the behavior of interdisciplinary care teams in hospital-based intrapartum care. We will consider generalizable principles and practice to center patients in their care from perspectives of racial equity, healing-centered engagement and trauma reduction, and medical ethics.
Maura Jones, MD is Chief Resident, UCSF Dept of OBGYN and Reproductive Sciences in the UCSF Obstetrics & Gynecology Residency Program. She is a native of Monroe, Louisiana. She received her undergraduate degree (B.S. in Biology) from Xavier University of Louisiana and went on to receive her Medical Degree from Louisiana State University School of Medicine, in New Orleans. She is a proud first-generation college student, and the first physician in her family. On completion of residency, she will matriculate into the Maternal-Fetal Medicine Training program at the University of North Carolina- Chapel Hill. Her research and clinical interests are Health Equity, Mentorship/Support within undergraduate and graduate medical education with a focus on historically and contemporaneously excluded groups, and Quality Improvement.
Deb Borne, MD, MSW is with the San Francisco Department of Public Health. Her focus is on Health Policy, Vulnerable Populations and People Experiencing Homelessness. Deb obtained her master’s degree in social work at Columbia University, attended medical school at Brown University and completed residency training in Family and Community Medicine at UCSF. Over the past two decades, Deb has served highly marginalized communities in San Francisco as a social worker and physician. She cares for people living with complex medical, social and behavioral needs including HIV and hepatitis, substance use disorders and serious mental illness, homelessness, trauma, incarceration and community re-entry. Deb leads and teaches across SFDPH and UCSF on a range of topics including HIV prevention and risk reduction, healing-centered engagement, reducing medical trauma, and best practices in the care of people experiencing homelessness.
Jack Chase, MD, FAAHP FHM is Associate Professor, UCSF Department of Family and Community Medicine & Co-Chair, SFGH Ethics Committee. Jack is a faculty member at the UCSF Family and Community Medicine Residency Program based at SFGH, where he provides clinical care on the Social Medicine team, Family Medicine Inpatient Service, Supportive and Palliative Care Service, and Minor Procedure Clinic. As Co-Chair of the SFGH Ethics Committee, Jack supports ethics consultation, education and policy recommendations at SFGH and in SFDPH. He also serves on the leadership team for SFGH Social Medicine which provides interdisciplinary care to people experiencing substance use disorders, mental illness, homelessness, food insecurity, trauma, medical-legal and financial needs in partnership with SF Department of Public Health, SF City and County agencies and community-based organizations.
April 1, 2022 - "The National Clinician Consultation Center: 30 years (and counting) of tele-consultation for provider capacity-building and public health service"





The National Clinician Consultation Center (NCCC) is a unique, federally-supported educational resource of the Ryan White HIV/AIDS Program which has continually adapted since the early 1990s to address evolving health care needs of HIV-affected communities. Its team has provided over 313,000 consultations to clinicians across the U.S., and it has contributed to the growth and development of several notable initiatives including an international community dedicated to the intersection of reproductive health and infectious diseases as well as multi-disciplinary educational collaborations across medicine, nursing, and pharmacy. This presentation will include a brief history of the NCCC, recent and future expansion highlights, and perspectives from several team members.
Dr. Ron Goldschmidt, DFCM Professor and Vice Chair, is a seasoned family physician who founded the National Clinician Consultation Center (NCCC). Dr. Goldschmidt has served as member of multiple national advisory and review committees for HRSA, AMA, and AAFP in addition to publishing several manuscripts on HIV care. In 2005, Dr. Goldschmidt received the 2005 Kaiser Award for Excellence in teaching from UCSF.
Brenda Goldhammer, Program Director, has worked in the HIV, viral hepatitis, and substance use fields for over 30 years. As NCCC Program Director, she provides operational and strategic leadership and also serves as a principal liaison in the development of collaborative partnerships and public relations at the local, regional, and national levels. Ms. Goldhammer received her MPH from the University of California at Los Angeles, where she received the Improving Public Health in Southern California Fellowship and University Fellowship for academic excellence.
Dr. Betty Dong, Professor of Clinical Pharmacy and Family and Community Medicine, is a senior HIV and viral hepatitis consultant with the NCCC. She is a prolific clinical educator, and has also published numerous manuscripts and book chapters on HIV and hepatitis C pharmacotherapy. She is the distinguished recipient of the 2019 Daniel B. Smith Practice Excellence Award from the American Pharmacists Association.
Dr. Christine Pecci, Professor of Family and Community Medicine and NCCC Women and Children’s Health Consultant, is a family physician and clinician educator with maternal health expertise who provides consultation on perinatal HIV for the NCCC.
Dr. Carolyn Chu is a family physician and HIV specialist. Prior to joining the NCCC, she served as medical director for a network of federally-qualified health centers in New York City. She is an experienced clinician educator and has investigated the integration and effectiveness of HIV medical services in community-based and primary care settings.
March 4, 2022 - "Afghan Clinic: Barriers to Health for Afghan Refugees & How We Can Address Them"


The last four decades of turmoil in Afghanistan are responsible for one of the worst episodes of forced displacement in world history. Nearly six million Afghans have been forcibly displaced from their homes, leaving them at risk of poor health. Afghan Clinic is a public health initiative by and for Afghan refugees. In this talk, we discuss findings from interviews with Afghan refugee women and community organizers who serve them. We conclude with recommendations on serving Afghan refugee patients and mitigating their barriers to health and healthcare.
Nazineen Kandahari, MS is a student in the UCSF Program in Medical Education for the Urban Underserved. As an Afghan refugee, Nazineen intimately experienced how the healthcare institution in the United States was not built to serve certain people. Thus from a young age, she committed herself to promoting people’s agency. Through community service, research, and public health intervention work, Nazineen has established herself as a trusted leader within the refugee community. She is passionate about health equity and community engagement. Nazineen is currently the Principal Investigator of a community-based health intervention for forcibly displaced Afghan immigrant women. She completed her Master of Science at the UC Berkeley School of Public Health on a study exploring the sexual health needs of Arab immigrant youth. Nazineen was named a “Student Who Rocked Public Health in 2021” by the Journal of Public Health Management & Practice and is a UC Berkeley School of Law Human Rights Center Fellow and Albert Schweitzer Fellow.
Nilufar Kayhani is an undergraduate student studying Public Health at the University of California, Berkeley. Nilufar is the child of Afghan refugees and is committed to resolving health inequities, particularly those experienced by refugees. She has initiated multiple community-based participatory research projects with historically marginalized populations while at UC Berkeley. She is currently a research intern at the Srivastava Lab at the Gladstone Institutes at the University of California, San Francisco. Nilufar is a pre-medicine student passionate about public health.
February 4, 2022 - "Family Medicine and Abortion: Responding to the Evolving Crisis in Access to Reproductive Health Care"



Family medicine’s core values include continuity of care, meeting patients’ and communities’ needs, care across the life course, and social justice. Abortion care is clearly aligned with these values, particularly in the current political and legislative climate, where access to abortion is increasingly limited and abortion care increasingly stigmatized. In this presentation, we will discuss the current state of abortion access, in California and the US as a whole, and will then review research done with new career family physicians about how they understand the values of our specialty and how this understanding relates to their decision making about abortion care. We will then discuss current initiatives to train and support family physicians to provide abortions. We will conclude with a panel discussion about how family physicians and the specialty of family medicine can act on our values through abortion care provision and advocacy and take questions from the audience.
Christine Dehlendorf, MD, MAS is a family physician with fellowship training in Family Planning and a Master’s degree in clinical research. She is the director of the Person-Centered Reproductive Health Program in the Department of Family & Community Medicine at UCSF, which aims to advance reproductive autonomy and well-being by conducting research and designing programs that center people’s experiences and preferences for sexual and reproductive health and health care, guided by an attention to the intersecting oppressions and structural injustices that impact people’s lives and health. Her research includes the development, evaluation and dissemination of interventions to better meet people’s reproductive needs, and formative research to better understand people’s reproductive health care experiences and preferences. In addition to her research, she provides primary care and abortion services within the San Francisco Bay Area.
Lealah Pollock, MD is a family doctor who specializes in care for women living with HIV throughout their lives, including during pregnancy and the postpartum period. She is the Director of Women and Children's Consultation Services and the Perinatal HIV Hotline at the National Clinician Consultation Center, where she leads a team dedicated to helping providers around the country provide patient-centered and guideline-driven care to pregnant people with HIV and their families. She also provides primary and specialty care to female-identified and gender diverse people with HIV at UCSF and teaches and provides abortion services in the Bay Area. Dr. Pollock earned a master's degree in health and medical sciences at University of California, Berkeley and her medical degree from UCSF's joint medical program with UC Berkeley.
Montida Fleming, MD is a full spectrum family and community medicine doctor who has focused on comprehensive reproductive health care, addiction medicine, and gender affirming care. She is an Assistant Clinical Professor in the UCSF Family and Community Medicine Residency Program where she trains family physicians in hospital medicine, early pregnancy and prenatal care, addiction medicine, and abortion care. In addition to providing and teaching abortion care in the Bay Area, she previously traveled to low-resource and restricted abortion access areas to provide care. Dr. Fleming currently practices gender affirming care and medication abortion care across multiple states via telehealth. Outside of clinical care, she participates in media, legislative, and AAFP advocacy efforts to improve and expand access to comprehensive reproductive health care, reduce barriers, and promote reproductive justice. She received her MD from Sydney Kimmel Medical College at Thomas Jefferson University, and completed her residency at San Francisco General Hospital with the University of California, San Francisco.
January 7, 2022 - "Firearm Violence: Where We Stand, What We Can Do"

This presentation will review the basic epidemiology of firearm violence, assess current trends and their implications, and review options for preventive action by health professionals. It will focus on recent research and emphasize findings for California.
Dr. Wintemute is Distinguished Professor of Emergency Medicine and Baker–Teret Chair in Violence Prevention at the University of California, Davis. He is the 2022 UCSF Robert Crede Primary Care Lecturer, named in honor of one of UCSF’s first leaders of academic primary care. Dr. Wintemute is the founding director of the Violence Prevention Research Program at UC Davis and of the California Firearm Violence Research Center, the nation’s first publicly-funded center for research in this field, overcoming formidable political obstacles to developing and sustaining a major research program on gun violence as a public health emergency and effective approaches to firearm safety. He practices and teaches emergency medicine at UC Davis Medical Center. Trained initially as a biologist at Yale University, Dr. Wintemute attended medical school and family medicine residency at UC Davis and studied epidemiology and injury prevention at The Johns Hopkins University.
December 3, 2021 - “Who We Hire Matters: How Health Systems Address Structural Racism Through Hiring People With Histories of Incarceration”


Decades long policies of mass incarceration and criminalization of mental illness and substance use disorder have resulted in significant health disparities for individuals and communities impacted by the criminal legal system. While primary care health systems can play an important role in addressing these disparities, studies show that people face stigma and discrimination in health systems because of their incarceration history.
The Transitions Clinic Network (TCN) works with primary care clinics to transform their systems to improve health equity for communities impacted by the criminal legal system. Clinics participating in the TCN hire community health workers with lived experience of incarceration dismantling systems that have historically prevented people with criminal records from accessing employment in the health field.
Shira Shavit, MD is a Clinical Professor of Family and Community Medicine at the University of California in San Francisco and the Executive Director and co-founder of the Transitions Clinic Network (TCN). For over a decade through research and community engagement, Dr. Shavit has been redefining national best practices to address the health inequities experienced by communities impacted by mass incarceration. In addition to providing clinical care to communities impacted by incarceration, Dr. Shavit has led health system transformation in over 48 primary care systems in 14 states and Puerto Rico resulting in healthcare career opportunities for hundreds of people with criminal legal involvement as community health workers. Her work in the TCN has also been shown to cut health care and criminal legal costs, and support healthy, sustained integration of individuals returning home from incarceration. In 2012, she led a Center for Medicare and Medicaid Innovation funded project across 11 sites in collaboration with City College of California. She also worked as a consultant to reform healthcare systems in the California State prisons in collaboration with the Federal Receivership (2006-2011). She is a recipient of the Robert Wood Johnson Community Health Leader Award (2010). Dr. Shavit graduated from Washington University in St. Louis, completed her MD at Rush University in Chicago, and completed her residency training at the University of California, San Francisco. She is currently a California Health Care Foundation Health Care Leadership Fellow.
Joseph Calderon, CHW, Senior Community Health Worker at the Transitions Clinic Network. Joe is a native of San Francisco and at the age of 23 he started serving a life sentence. After nearly 20 years incarcerated, he began to explore ways to give back to society upon his release. He currently works as a the Senior CHW and trainer at the Transitions Clinic Network (TCN), a national organization dedicated to improving health and reentry outcomes for those returning to the community from incarceration. Joe trains and mentors CHWs with histories of incarceration who are employed by TCN programs nationwide. Joe was an appointee to the San Francisco Reentry Council from 2013-2016 and now serves on the Policy and Procedure Sub-Committee. He also served on the Equity Advisory Committee with the San Francisco Human Rights Commission. In 2017 the San Francisco Department of Health appointed Joe to the SF LEAD (Law Enforcement Assisted Diversion) Policy Committee. He has a passion for working with diverse and disenfranchised populations, leveraging his personal experience with incarceration to advocate for social justice and community investment. Mr. Calderon has a Post-Prison Community Health Worker certificate from San Francisco City College and plans on continuing his education in public health. Joe completed a JustLeadershipUSA fellowship in 2018.
November 5, 2021 - “Contextualizing Care: An Essential and Measurable Clinical Competency”

Evidence-based care plans can fail when clinicians do not consider a patient’s relevant life circumstances -- such as an inability to afford a medication, a competing responsibility, or a loss of social support -- when planning their care. The capacity to systematically identify and incorporate patient life context into medical decision making has been described as the process of contextualizing care. Based on an analysis of over 500 unannounced standardized patient simulations and 7000 audio recorded clinical encounters over the course of more than a decade, Dr. Weiner’s team has characterized the skills required to contextualize care, measured their effect on patient outcomes and health care costs, tested various strategies for teaching the skills and measuring performance, and established a contextualizing care QI program at several VA medical centers. His presentation will provide an overview of this work.
Saul Weiner, MD, is professor of medicine, pediatrics, and medical education at the University of Illinois at Chicago (UIC), and deputy director of the research Center of Innovation for Complex Chronic Health Care at the Veterans Health Administration. His research on contextualization of care has been supported by the Department of Veterans Affairs (Health Services Research & Development), the Agency for Healthcare Research and Quality, the Robert Wood Johnson Foundation, and the National Board of Medical Examiners. Dr. Weiner is the University of Illinois at Chicago 2013 Distinguished Researcher of the Year in the Clinical Sciences. He has served as medical education dean, university vice provost, and currently as senior advisor to the provost. His book, Listening for What Matters: Avoiding Contextual Errors in Health Care, published by Oxford University Press, received the 2017 American Publishers Award for Professional & Scholarly Excellence in the Life Sciences from the American Association of Publishers. His latest book is On Becoming a Healer: The Journey from Patient Care to Caring About Your Patients, published by Johns Hopkins University Press (April 2020).
For those of you interested in this body of work and its clinical and research implications, here is a new “fireside chat” series of short videos on contextualizing care:
https://youtube.com/playlist?list=PL9-b6XZZMupzmVuuwn1Ipph0dpI1fxx2d
October 1, 2021 - “Should We Screen for and Document Social Risk in Health Care Settings?”



Screening for adverse social determinants of health, or social risk factors, is becoming increasingly common in health care settings. This screening is supported by multiple professional societies, including the AAFP, AAP and ACP. There is growing evidence to support activities to identify and intervene on patient social risk factors, with the goal of improving patient health, wellness, and health equity. Researchers from UCSF SIREN will discuss 1) the acceptability of social risk screening from the perspective of patients and caregivers of pediatric patients, and 2) current screening activities at UCSF and ZSFG.
Dr. Emilia De Marchis is a family physician and health services researcher at the University of California, San Francisco. Her research is based out of the UCSF Social Intervention Research & Evaluation Network (SIREN), where she works to assess and improve how we screen for and address social risk factors within health care settings. Dr. De Marchis co-directs coursework through the UCSF Implementation Science Training program, Partnerships for Research in Implementation Science for Equity (PRISE) Center. She uses implementation science methods to focus on moving research on social risk screening, assistance and adjustment activities into real-world settings. Her clinical work is based out of the UCSF Family Medicine Center at Lakeshore. Through her research and clinical practice, she hopes to advance the health care system’s integration of patient social risk data to provide high quality, patient-centered preventative health care, to reduce health disparities. Dr. De Marchis received her MD from Stanford University, and her MAS in Clinical Research and Certificate in Implementation Science from UCSF.
Dr. Matt Pantell is an Assistant Professor at UCSF, where his research is conducted with the UCSF Center for Health and Community, the UCSF Social Interventions Research and Evaluation Network, and the UCSF Preterm Birth Initiative. His research focuses on the utility of incorporating social information into clinical decision making, addressing social needs in clinical settings, data mining and the analysis of large datasets, and biological manifestations of the social determinants of health. Clinically, Dr. Pantell works is as a pediatric hospitalist at UCSF Benioff Children's Hospital - Mission Bay and Washington Hospital in Fremont. He also works as a pediatric urgent care physician and runs the Tattoo Removal Clinic at Zuckerberg San Francisco General Hospital.
Dr. Caroline Fichtenberg is the Managing Director of the Social Interventions Research and Evaluation Network (SIREN) and Research Scientist in the Department of Family and Community Medicine at the University of California, San Francisco. In these roles, she leads efforts to conduct, catalyze, and disseminate high quality research on health sector strategies to reduce health inequities by addressing social determinants of health. She brings to these positions more than a decade of experience working to improve health and economic outcomes for America’s most vulnerable families, including seven years working on national efforts in Washington, DC. While Director of Research at the Children’s Defense Fund (CDF), she led the development of a report that identified nine federal policy changes that could reduce child poverty by 60 percent. As Director of Epidemiology and Planning at the Baltimore City Health Department, she oversaw the city’s first analysis of neighborhood health inequities that uncovered a 20-year gap in life expectancy between the richest and poorest neighborhoods of the city. Caroline also served as director of the Center for Public Health Policy at the American Public Health Association (APHA) and as Health Policy Advisor to Senator Harkin on the Senate Health, Education, Labor and Pensions committee, where she promoted health in all policies approaches to improve health outcomes and reduce health inequities. She earned her Ph.D. in Epidemiology from Johns Hopkins University, an M.S. degree in Biology from Yale University and an A.B. in Molecular Biology from Princeton University.
September 3, 2021 - “Redefining Global Health through Structural Competency and Allyship”


Unlike hypertension, the widely used term Global Health has very different meanings depending on where one stands: United States, Switzerland or Malawi. This highlights long standing differences in power and privilege, and the persistence of Global Health’s colonial roots. We however find ourselves in a time of opportunity to push for greater accountability and true partnership on the part of privileged countries and institutions. Doing so requires continuous self-study and the willingness to take personal and professional risks. We will discuss a structural competency framing of Global Health, and the challenges and rewards of pursuing true allyship as part of the larger struggle for dignity for all.
Sundeep K Gupta, MD, MPH, DTMTH, is a FCM faculty member at Natividad Medical Center; he is a past CDC Country Director for Uganda, Malawi and Zambia. He is also an Assistant Clinical Professor in the Division of Infectious Diseases at UCLA. Dr. Gupta completed his BS in Political Science, MD and MPH from Northwestern University, and went on to complete his residency in Family Medicine at Natividad Medical Center. After completing his DTMTH at Tulane University, Dr. Gupta joined CDC’s Epidemic Intelligence Service ‘disease detective’ program. Over the subsequent 12 years, he worked for CDC in 12 countries in Africa, Asia and Central America, leading responses to HIV, Ebola and other epidemics, while working in partnership with host country colleagues to strengthen public health systems. Dr. Gupta was subsequently seconded by UCLA to Partners in Hope, a local Malawian organization, to lead their efforts to fight the HIV epidemic. Dr. Gupta is board certified in Family Medicine by the American Board of Family Medicine. He has published over 50 manuscripts and provided public health leadership across different cultures and types of public health systems across the globe. His professional interests include patient lived experience, HIV primary care, community medicine, equity and social accountability, applied epidemiology and public health. His personal interests include hiking, biking and spending time with his family.
Professor Address Mauakowa Malata PhD, MSc, BSc, FAAN. is the Vice-Chancellor of Malawi University of Science and Technology, former President of Africa Honor Society of Nursing of Sigma Theta Tau International; former Vice President, International Confederation of Midwives, former Principal of Kamuzu College of Nursing and spearheaded it to become a World Health Organization Collaborating Centre for Inter Professional Education and Leadership in 2016. A renowned international speaker, author and editor of various journals in the field of health, nursing, midwifery, and health workforce, she serves on various international, regional and national boards. Dr. Malata is an advocate for girls and women empowerment through education. Her research work focuses on maternal and newborn health, quality of care, health workforce and innovation and technology. She is a Virginia Henderson Fellow of Sigma Theta Tau International (STTI), an Adjunct Professor at Michigan State University, a Fellow of the American Academy of Nursing (FAAN); a Global Health Fellow at University of California San Francisco University; an Adjunct Professor in the Department of Obstetrics and Gynecology, Baylor College of Medicine. She was awarded a Doctor Honoris Causa by University of Oslo in Norway, 2018 ECU Distinguished Alumni and ECU Honorary Award of Doctor of Nursing honoris causa, 2019 in Australia.
August 6, 2021 - “Addressing Racism and Advancing Health Equity In and Beyond the Exam Room”

Racism and the repeated trauma of experiencing racism has a direct impact on health and detrimental effects on our individual patients, our communities, and our society. In primary care, we are poised to lead action and meaningful anti-racism change because we understand our patients not just in terms of their pathophysiology, but also in terms of their relationships, their experiences, their communities, and their social context. We will discuss actions we can take in our own practices with our patients, communities, and even beyond to address racism, advance health equity, bring about change, and promote justice.
Tricia C. Elliott, MD, FAAFP is the immediate past president of the Society of Teachers of Family Medicine and a past president and past board chair of the Texas Academy of Family Physicians. She graduated from Rice University and received her medical degree from University of Texas Medical Branch. She went on to complete her residency in Family Medicine at Albert Einstein/Montefiore Medical Center Residency Program in Social Medicine. Dr. Elliott is board certified in Family Medicine by the American Board of Family Medicine. She has over twenty years graduate medical education (GME) experience which includes nationally-recognized work with the ACGME Family Medicine Milestones group, the American Academy of Family Physicians Council on Education, and the Society of Teachers of Family Medicine. She has provided administrative and clinical leadership across various types of health systems, including academic medical centers, a multi-specialty group practice, and a community-based, university-affiliated teaching hospital, in the roles of clinical faculty, program director, Vice Chair for Clinical Affairs, and currently as Senior Vice President of Medical Staff, Academic, & Research Affairs/Chief Academic Officer/DIO at JPS Health Network in Fort Worth, Texas.
She is Professor in Family Medicine at Texas Christian University/University of North Texas Health Sciences Center (TCU/UNTHSC) School of Medicine, Affiliate Professor at UNTHSC Texas College of Osteopathic Medicine, and Adjunct Professor at University of Texas Medical Branch School of Medicine. Dr. Elliott’s academic interests include graduate and undergraduate medical education, learner assessments, health care advocacy and policy, and leadership development and mentoring. Her clinical interests include primary prevention, chronic disease management, women’s health, migraine management, ambulatory procedural training, patient education, and community medicine. Her personal interests include singing/vocal performance, collecting art, cooking, dancing, public speaking, and travel.
June 4, 2021 - “Strange Bedfellows: Adventures in the Science, History, and Surprising Secrets of STDs”
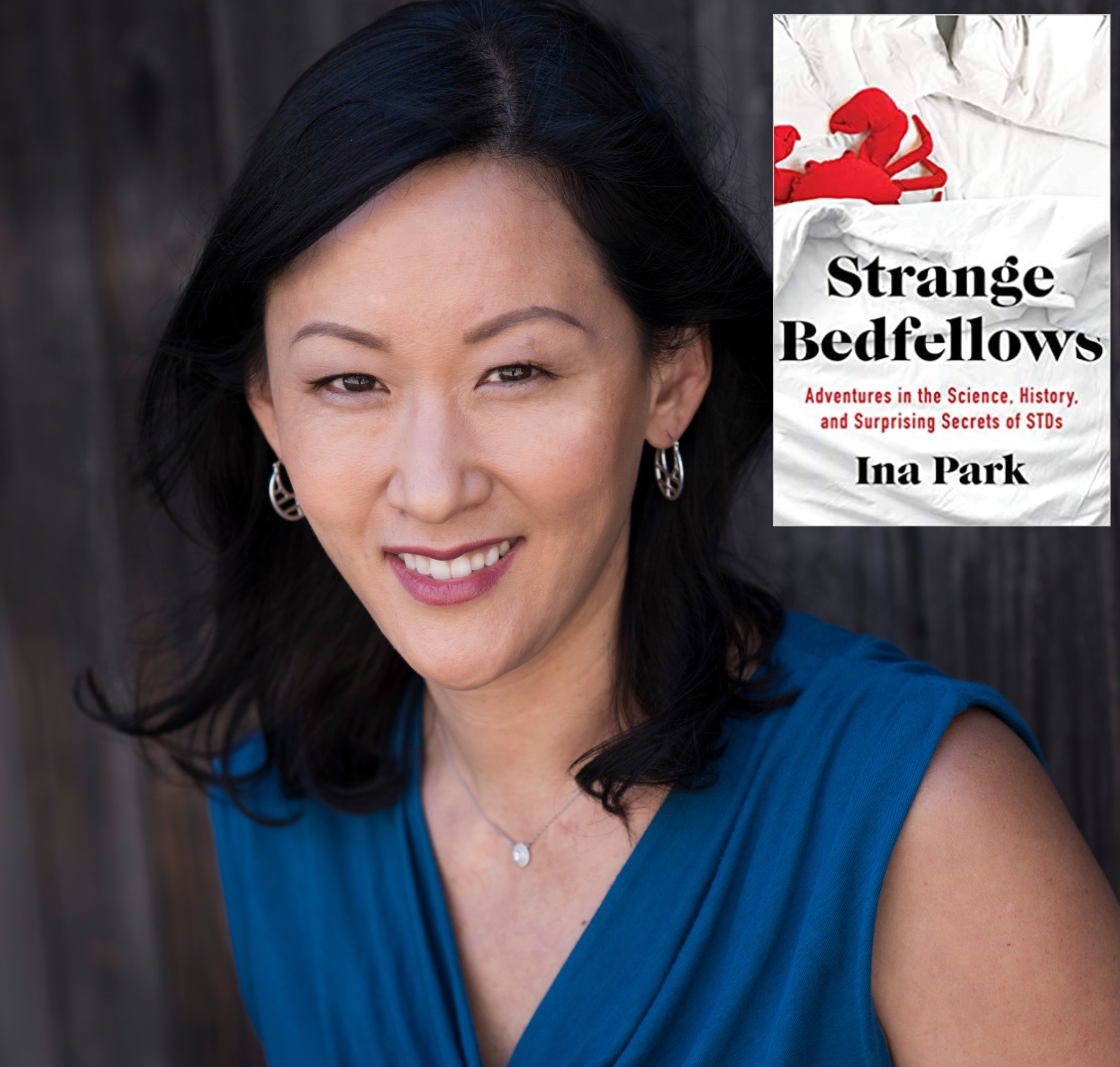
Sexually Transmitted Infections (STIs) have been hidden players in our lives for the whole of human history, affecting everything from World Wars to the gay rights movement. But despite their prominence, STIs have been thought of as curious – and often terrifying – taboos for centuries, which begs the question: why do we know so little about them?
Join us for Family and Community Medicine Grand Rounds with Ina Park, MD, MS who will talk about her new book Strange Bedfellows: Adventures in the Science, History, and Surprising Secrets of STDs. She'll share stories of real people’s sexual escapades and historical tales, along with the latest science of STI and HIV prevention, venturing beyond the bedroom to examine the role that STIs have played in our lives and society. Hailed by The New York Times as “joyful and funny” Strange Bedfellows has been praised for its use of “compassion, science and a loving playfulness” to diffuse the stigma surrounding these common infections.
INA PARK MD, MS, is an associate professor at the UCSF School of Medicine in the Departments of Family and Community Medicine and Obstetrics, Gynecology, and Reproductive Services, Medical Consultant at the Centers for Disease Control and Prevention, Division of STD Prevention, and Medical Director of the California Prevention Training Center. Recently, Dr. Park served as a co-author of the 2021 CDC STI Treatment Guidelines and contributor to the Department of Health and Human Services first STI National Strategic Plan. In addition to her current book, her writing has also appeared in the New York Times.
May 7, 2021 “Social Policies to Address Health Inequities: Harder Than It Looks”

There is generally positive but occasionally conflicting evidence on the health benefits of social and economic policies to address social determinants of health like poverty and educational attainment. Dr. Rita Hamad will delve into research to understand the possible reasons for the conflicting results, including the possibility that well intentioned policies may have negative effects. She will highlight the importance of evaluating the effects of even the most commonsense policies, in order to inform the design of future interventions to address the social determinants of health.
Dr. Rita Hamad is an Associate Professor at UCSF. She is a social epidemiologist and family physician in the Department of Family & Community Medicine and the Philip R. Lee Institute for Health Policy Studies. She is the director of the Social Policies for Health Equity Research Program, and Associate Director of the Center for Health Equity. Her research focuses on the pathways linking poverty and education with health disparities across the life course.
Watch recording here: https://youtu.be/0sgEkJZttvE
April 2, 2021: "Achieving Racial and Ethnic Equity in COVID-19 Vaccination: Learnings from Community Based Participatory Research."
UCSF faculty, staff, and community partners leading the STOP COVID-19 CA Project will discuss learnings from focus groups and interviews with members of the Black/African American, Latinx, and Chinese/Chinese American communities about perspectives on COVID-19 vaccination.
To view this presentation please see the links below.
Internal UCSF users: https://ucsf.box.com/s/a9ui8lpssjuaydmt5omh9s2yngzt28q4
External users: https://youtu.be/rUydOpWnCLs
March 5, 2021: "Lancet Commission on Public Policy and Health in the Trump Era"

Presentation by Dr. Kevin Grumbach and Dr. Julianna Morrison discuss the newly released report of the Lancet Commission on Public Policy and Health in the Trump Era, recommendations to put the US back on the path to health for all, and discuss the implications for the policy agenda of the Biden administration and new Congress.